Reinventing Comfort: Innovative Practices in Pain Treatment Clinics
The Evolving Landscape of Pain Relief Centers
Chronic pain is no longer a side note in healthcare. It is a massive, unrelenting weight dragging down productivity and quality of life for millions of adults. The outdated approach of handing out prescriptions and sending patients on their way is crumbling. In its place, high-performing clinics are adopting sharper, patient-focused models that treat the individual, not just the symptom. These centers are rethinking every layer of care, from faster diagnostics to integrated recovery plans that merge science and empathy. Multidisciplinary teams, precision diagnostics, and data-informed strategies are replacing guesswork. It’s an evolution born from necessity, and one that refuses to accept pain as an unavoidable fact of aging or injury.
Digital Health Tools in Today’s Pain Therapy Clinics
A wave of digital innovation has swept into the exam room. Wearable sensors track joint movement and sleep cycles. Mobile apps record pain flare-ups with time-stamped precision. Virtual-reality modules trick the brain into relaxing its pain signals. AI-powered diagnostics mine months of data in seconds, spotting patterns that human eyes overlook. This real-time feedback gives patients a stake in their recovery while giving clinicians hard evidence to guide adjustments. The result is less guessing, faster course corrections, and fewer bursts of unchecked pain. Technology isn’t replacing the human touch here. It’s sharpening it.
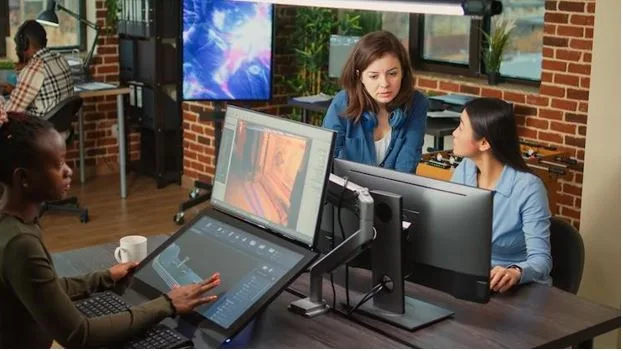
Multidisciplinary Collaboration at Chronic Pain Control Facilities
In top clinics, the days of siloed treatment are over. Physical therapists focus on mobility. Psychologists tackle the emotional fallout. Pharmacists guide safe medication strategies. Pain physicians orchestrate the big picture. When these specialists sit in the same room, comparing notes, the patient becomes more than a case number. Cross-discipline meetings streamline decisions and shorten the lag between problem and solution. The outcome is care plans that are leaner, faster, and better aligned with the patient’s life. This is not teamwork for show. It’s a practical method to wring inefficiency out of a complex process.
Integrative Techniques at Modern Pain Assistance Clinics
A growing number of clinics are leaning into therapies once considered fringe. Acupuncture sessions that reduce nerve sensitivity. Mindfulness training to cut the loop between stress and flare-ups. Nutritional guidance targeting inflammation. Skilled therapeutic massage to revive circulation. These are not replacements for conventional medicine but smart companions. The data is mounting. Lower opioid dependence, faster recovery milestones, stronger patient-reported satisfaction. By weaving these integrative techniques into the standard regimen, clinics are building treatment plans that hit more angles and satisfy more patients.
Leveraging Patient Data with Advanced Analytics at Pain Care Facilities
Every clinic collects data. Not every clinic uses it well. The most advanced pain facilities are funneling massive datasets into algorithms built for prediction and prevention. Machine-learning models can flag a patient whose symptoms are likely to spiral weeks before damage is done. This means less trial-and-error medication dosing, fewer ER visits, tighter care loops. Outcome tracking is no longer a bureaucratic checkbox. It’s a living map of a patient’s progress, ready to be adapted in real time. Personalization here is not a marketing slogan. It’s math meeting medicine.
The Vital Role of Telemedicine in Contemporary Pain Relief Practices
The value of remote access is obvious for someone who can’t easily leave home. Virtual consultations allow clinicians to see the home environment, spot hazards, and deliver targeted advice. Telehealth assessments keep rural patients from driving hours for a check-in. Digital platforms let physicians adjust prescriptions or physical therapy routines between in-person visits without losing continuity. This blended model opens the clinic’s reach and preserves energy for people already battling fatigue. Technology here doesn’t dilute care quality. It removes barriers that have lingered for decades.
Establishing Trust: The Human Touch in Clinical Pain Services
No amount of software or analytics can replace trust. In a pain management clinic, genuine connection still drives results. Patients respond to clear language instead of medical jargon. They adhere when they understand the reasoning, not just the instruction. Empathy—measured, specific, rooted in reality—reduces fear and builds commitment to the plan. Shared decision-making flips the script from passive patient to active partner. Clinics that get this right see fewer no-shows, deeper engagement, and better outcomes because the relationship itself becomes part of the therapy.
Charting the Next Frontier in Pain Care
Regenerative medicine is inching toward mainstream use, offering the possibility of rebuilding damaged tissues instead of just calming them. Neurostimulation implants are becoming smaller, more precise, more controllable. Virtual coaching bots could soon deliver 24/7 motivational nudges backed by live data from wearable devices. The next era may treat pain before it blooms, using predictive AI to preempt triggers through targeted lifestyle shifts and preventive therapies. Research pipelines are brimming with options that could redefine the ceiling of what’s possible. The future of pain care isn’t distant. It’s already leaking into the present, reshaping expectations for what patients should demand and what clinics must deliver.