GERIATRICS Heart Failure Overview and Definition
As populations around the world continue to age, the burden of cardiovascular diseases among older adults has increased significantly. One of the most common and complex conditions affecting the elderly is GERIATRICS Heart Failure Overview and Definition, a topic that deserves clear explanation, awareness, and timely intervention. Heart failure in geriatric patients is not just a single disease but a clinical syndrome that results from structural or functional impairment of the heart, leading to inadequate blood flow to meet the body’s needs.
Unlike younger individuals, older adults often present with multiple chronic conditions, making diagnosis and management more challenging. Understanding the clinical background, risk factors, and treatment approaches of heart failure in geriatric patients is essential for patients, caregivers, and healthcare professionals alike.
Understanding Heart Failure in the Elderly
Heart failure does not mean that the heart has stopped working. Instead, it means the heart is unable to pump blood efficiently enough to support normal bodily functions. In older adults, this condition often develops gradually and may be overlooked due to overlapping symptoms with aging or other illnesses.
The heart may fail in two main ways:
- Systolic heart failure, where the heart muscle cannot contract effectively
- Diastolic heart failure, where the heart becomes stiff and does not fill properly
In geriatric patients, diastolic dysfunction is particularly common due to age-related changes in the heart muscle and blood vessels.
Definition of Geriatric Heart Failure
GERIATRICS Heart Failure Overview and Definition refers to heart failure occurring in individuals typically aged 65 years and older, characterized by reduced cardiac output, fluid retention, and decreased physical tolerance. What differentiates geriatric heart failure from heart failure in younger adults is the presence of multiple comorbidities, frailty, and polypharmacy.
Conditions such as hypertension, diabetes, kidney disease, and chronic lung disorders frequently coexist and influence both diagnosis and treatment outcomes. Cognitive decline and limited mobility may further complicate disease management.
Common Causes and Risk Factors
Several factors contribute to the development of heart failure in elderly individuals. Some of the most common causes include:
- Long-standing high blood pressure
- Coronary artery disease
- Previous heart attacks
- Heart valve disorders
- Age-related structural heart changes
Secondary risk factors such as obesity, sedentary lifestyle, smoking history, and poor dietary habits also play a role. In geriatric populations, even mild infections or dehydration can trigger heart failure exacerbations.
Signs and Symptoms to Watch For
Recognizing heart failure early is critical, yet symptoms in older adults can be subtle. Common warning signs include:
- Shortness of breath during routine activities
- Swelling in the legs, ankles, or abdomen
- Fatigue and weakness
- Rapid or irregular heartbeat
- Difficulty sleeping flat due to breathing discomfort
Secondary symptoms such as confusion, loss of appetite, and sudden weight gain may also appear, particularly during acute episodes.
Because these symptoms often mimic normal aging or other chronic conditions, many geriatric patients are diagnosed later than ideal.
Diagnostic Approach in Geriatric Patients
Diagnosing heart failure in elderly individuals requires a comprehensive approach. Physicians typically rely on:
- Detailed medical history and physical examination
- Blood tests to assess cardiac markers
- Imaging studies such as echocardiography
- Electrocardiograms to evaluate heart rhythm
Specialized geriatric care centers, such as Liv Hospital , emphasize a multidisciplinary approach, combining cardiology, geriatrics, and rehabilitation services to ensure accurate diagnosis and personalized treatment plans.
Clinical Management and Treatment Strategies
Treatment of heart failure in geriatric patients focuses on improving quality of life, reducing hospitalizations, and slowing disease progression. Management strategies often include:
- Medications to reduce fluid overload and control blood pressure
- Lifestyle adjustments tailored to physical ability
- Monitoring for medication side effects due to age-related changes in metabolism
Unlike younger patients, elderly individuals may require lower medication doses and closer monitoring. Secondary considerations such as kidney function, fall risk, and cognitive health are always taken into account.
For more detailed medical insights and specialized care options, patients and caregivers can explore GERIATRICS Heart Failure Overview and Definition , which provides focused information specifically designed for aging populations.
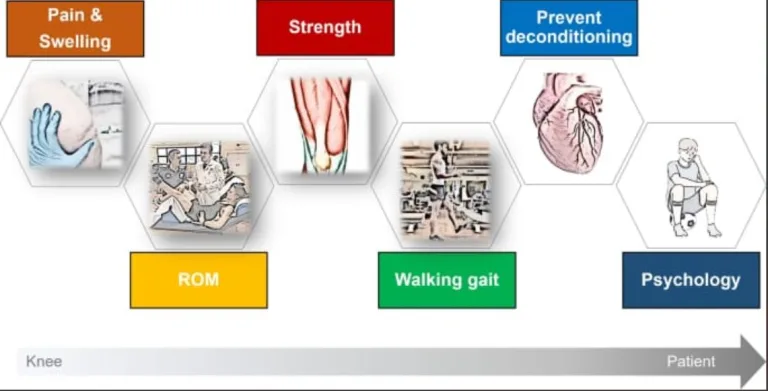
The Role of Rehabilitation and Supportive Care
Beyond medications, supportive therapies play a critical role in managing geriatric heart failure. Cardiac rehabilitation programs, when adapted for older adults, can improve endurance, balance, and confidence.
Nutritional counseling is equally important. Older adults often struggle with maintaining a heart-healthy diet due to appetite changes or dental issues. Caregiver education also helps ensure medication adherence and early detection of worsening symptoms.
Impact on Quality of Life
Heart failure significantly affects independence and daily functioning in older adults. Tasks that were once simple—such as walking short distances or climbing stairs—may become exhausting. Emotional health can also be impacted, with anxiety and depression being common secondary challenges.
This is why a holistic approach is essential. Treating the heart alone is not enough; emotional well-being, mobility, and social support must also be addressed to achieve meaningful outcomes.
Prevention and Early Intervention
While aging itself cannot be prevented, many risk factors for heart failure can be managed. Regular health screenings, blood pressure control, and timely treatment of heart disease can delay or even prevent the onset of heart failure.
Maintaining physical activity, even at low intensity, supports cardiovascular health. Simple habits such as staying hydrated, managing stress, and following medical advice consistently can make a significant difference over time.
Looking Ahead: Living Better With Heart Failure
Living with heart failure in later years requires adjustments, but it does not mean life must stop. With proper medical care, lifestyle modifications, and emotional support, many elderly patients continue to live fulfilling lives.
In the final stages of care planning, focusing on overall well-being becomes just as important as clinical treatment. Resources that promote balanced living, gentle activity, and mental wellness—such as live and feel can offer valuable inspiration for maintaining a positive and mindful lifestyle alongside medical care.